Scientists at USC have developed a groundbreaking AI tool called RED (Rare Event Detection) that identifies cancer cells in blood samples within minutes. Learn how this innovation could transform early diagnosis and cancer care.
Discover How AI Is Changing Cancer Detection in Blood Samples: Inside the New “RED” Breakthrough
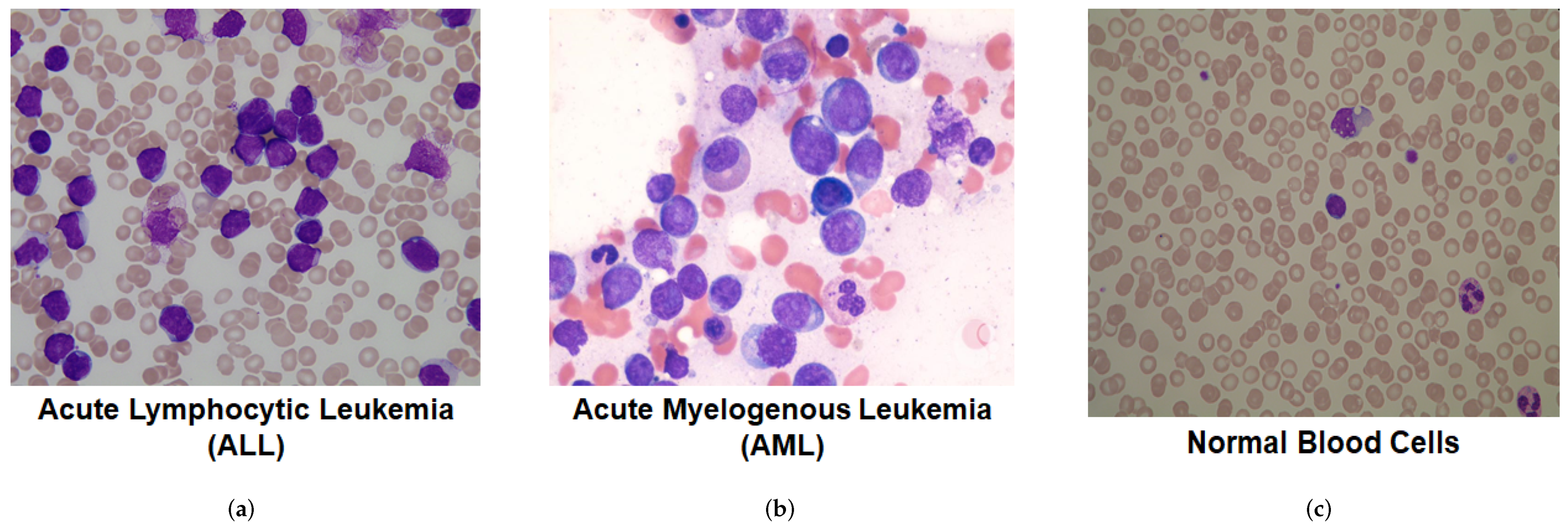
In laboratories around the world, scientists still spend countless hours peering through microscopes, searching for rare cancer cells hidden in blood samples — a task as daunting as finding a needle in a haystack. Now, artificial intelligence is reshaping that process.
Researchers at the University of Southern California (USC) have developed a new AI tool that can automatically identify cancer cells in blood samples, cutting analysis time from hours to minutes while improving accuracy. The system, called RED (Rare Event Detection), represents a major leap forward in how doctors might one day detect and monitor cancer without invasive biopsies.
The Challenge: Finding the Invisible
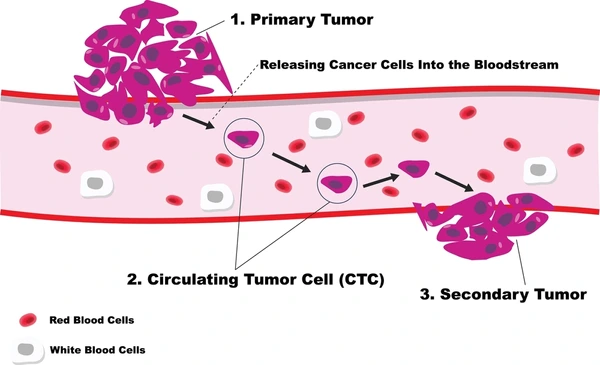
Cancer cells circulating in the bloodstream — known as circulating tumor cells (CTCs) — carry vital information about the disease’s presence and progression. But detecting them is notoriously difficult. A single milliliter of blood can contain billions of healthy cells and perhaps only a handful of malignant ones.
Traditionally, trained specialists must analyze these samples manually, scanning thousands of microscopic images to identify anomalies. The process is slow, expensive, and vulnerable to human fatigue. That’s where AI comes in — offering the speed and precision that humans alone can’t achieve.
Introducing RED: The AI That Finds the “Rare”
The RED algorithm takes a fundamentally different approach from conventional machine learning systems. Instead of being trained only on examples of cancer cells, it is designed to seek out anything unusual or rare within a dataset — much like an expert who instantly notices something out of place in a familiar environment.
Using advanced image analysis and anomaly-detection techniques, RED can analyze millions of blood-cell images and rank them by how different each one looks from the rest. The most “rare” cells are then flagged for review by scientists, dramatically reducing the amount of data they must manually inspect.
In recent lab studies, the system achieved striking results — detecting up to 99% of epithelial cancer cells and 97% of endothelial cells added to blood samples. Even more impressive, it reduced the number of images needing review by a factor of 1,000, while identifying twice as many promising candidate cells compared with traditional manual screening.
Why It Matters
Early and accurate cancer detection saves lives. Liquid biopsies — tests that look for cancer DNA or cells in blood — are among the most promising frontiers in oncology. Yet one of the biggest obstacles has been the difficulty of identifying these rare cells reliably and at scale.
RED’s ability to spot anomalies automatically could revolutionize how labs and hospitals conduct cancer screening, recurrence monitoring, and even treatment evaluation. By accelerating sample analysis, doctors could receive critical insights faster — potentially catching cancer before symptoms appear or before it spreads further.
How RED Works (Simplified)
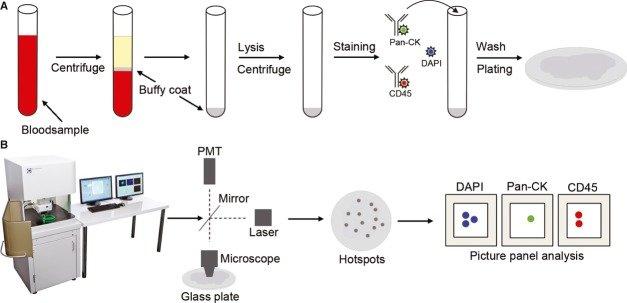
Behind RED’s simplicity lies sophisticated computer vision and machine learning. The system operates through several key stages:
-
Image Capture: High-resolution microscopes scan patient blood samples.
-
Preprocessing: The images are cleaned, standardized, and segmented so each cell can be analyzed individually.
-
Feature Extraction: The AI converts visual data into mathematical patterns, encoding each cell’s unique shape, texture, and color profile.
-
Rarity Scoring: Using anomaly-detection algorithms, it assigns a “rarity score” to every cell, ranking them from most typical to most unusual.
-
Human Review: Only the top-ranked rare cells — those most likely to be cancerous — are presented to experts for confirmation.
This approach eliminates the need for predefined templates or manual labeling of cancer cells, making the system more flexible and adaptable to new data.
Beyond the Microscope: Broader Implications
USC’s team believes RED could extend well beyond detecting circulating tumor cells. Early tests show promise in identifying other rare cell types linked to diseases like multiple myeloma or pancreatic cancer. The researchers also envision its use in other biomedical fields — from analyzing pathogens to studying immune cells.
More importantly, RED demonstrates how AI can complement, not replace, human expertise. By handling the repetitive, data-intensive work, it allows scientists to focus on interpretation and decision-making — the areas where human judgment still matters most.
Challenges and Limitations
While the technology’s potential is clear, important questions remain. How will RED perform in real-world clinical settings with highly variable samples? Can it maintain accuracy across different equipment, staining techniques, and patient populations?
Like any AI system, RED also faces issues of generalization and explainability. Clinicians will need confidence that its decisions are transparent and reliable. Moreover, large-scale validation, regulatory approval, and ethical oversight will be essential before hospitals can deploy it routinely.
The Future of AI in Cancer Detection
The success of RED hints at a broader future where artificial intelligence transforms every step of cancer care. As AI systems become better at understanding biological images, they could combine data from multiple sources — genetic sequencing, imaging, patient history — to deliver more comprehensive diagnoses.
Future versions might even use explainable AI models that not only detect anomalies but also visualize why a particular cell looks suspicious. Combined with advances in high-throughput imaging and cloud computing, such systems could one day make real-time cancer monitoring as simple as a routine blood test.
Key Takeaways
-
RED (Rare Event Detection) is an AI tool that can automatically detect rare cancer cells in blood samples within minutes.
-
It identifies anomalies rather than relying on pre-labeled data, making it adaptable to new diseases.
-
Early studies show up to 99% detection accuracy and 1,000× faster review speed.
-
The technology could transform early detection, monitoring, and treatment decisions in oncology.
-
Clinical validation, explainability, and ethical safeguards will be crucial for its future success.
Final Thoughts
The idea that a computer could find a single cancer cell hiding among millions of healthy ones once sounded like science fiction. Now, it’s quickly becoming reality. Tools like RED illustrate how artificial intelligence isn’t just changing technology — it’s redefining medicine itself.
As research continues, the hope is that AI-driven diagnostics will move from the lab into hospitals worldwide, offering faster, less invasive, and more accurate ways to detect disease. The “needle in the haystack” might not be so elusive for much longer.